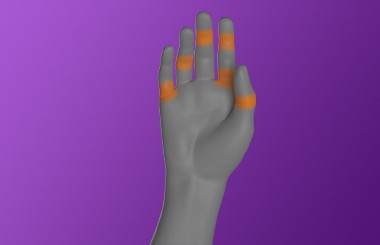
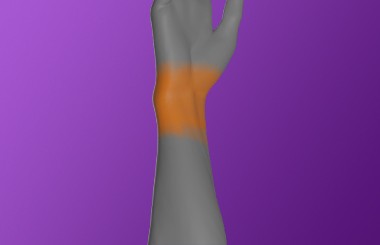
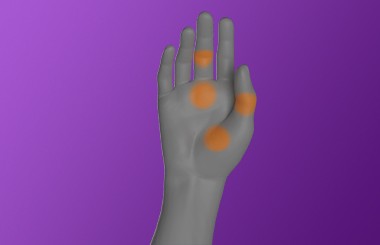
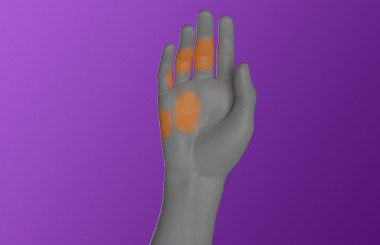
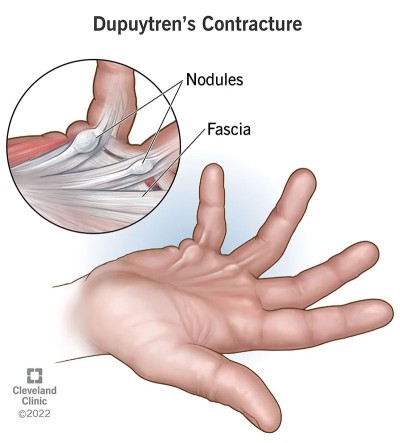
Hand and wrist pain can arise after an injury (e.g a fall), or develop with no known injury (e.g a flare of arthritis). Common reasons include aggravation of muscles, tendons, ligaments, arthritis in the joints and/or irritation of nerves.
You should see your doctor if you:
- Have pain that doesn’t show any signs of improvement, within a couple of weeks of self help
- Have pain that has rapidly deteriorated or suddenly worsened despite self help
- Have a history of inflammatory arthritis, immuno-suppression, cancer, Tuberculosis (TB), drug abuse, AIDS or other infection
- Feel unwell, have a fever, or unexplained weight loss
- Are experiencing significant and regular changes to your usual sleeping pattern
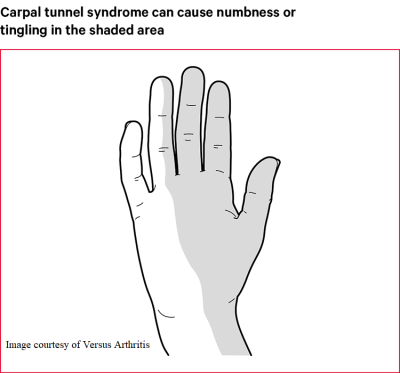
- You have any tingling or loss of sensation in your hand or wrist
- You notice changes to your grip strength and are frequently dropping things
- You have severe pain after trauma, such as a fall, collision, or impact to the wrist or hand
If you do not have any of the above, you may be able to effectively self manage your condition.
There are several ways you can help yourself including:
- Taking pain medication
- Keeping active - find a balance between rest and some activity, try not to overdo things (alter activities that make it worse so they are less painful)
- Using cold treatment, eg. ice packs, or heat treatment, eg. heat packs.